By Maria Soledad Hershey and Miguel Ruiz-Canela
Diet and physical activity (PA) are two of the most frequently addressed modifiable lifestyle risk factors, which increase morbidity and mortality from lifestyle diseases, including cardiovascular disease, obesity, type 2 diabetes, and some cancers. Hand-in-hand, diet and PA are frequently recommended in clinical practice for general health promotion, weight loss or weight maintenance, chronic disease prevention, and increased quality of life.1 Diet and PA are also considered multidimensional variables that can influence each other.2 Even the Mediterranean Diet (MedDiet) Pyramid underlines the importance of PA and other lifestyle factors beyond diet.3,4 Furthermore, evidence already suggests that greater adherence to both the MedDiet and PA is associated with better health biomarkers, lower risk of disease, and lower mortality when compared to the MedDiet or PA alone.5–9 While existing literature supports that a healthy MedDiet pattern and PA may be more effective when acting in combination rather than separately, questions still remain on exactly how, to what extent, and to whom is this combined effect most beneficial to target interventions in public health. Little has been studied on the a priori analysis of the interaction between diet and PA to determine its impact on hard clinical events or mortality thus far.10,11

In this hybrid study, we first present a comprehensive review of exiting studies on the combined effect between the MedDiet and PA on all-cause mortality to report the presence of interaction analyses. This was followed by an original analysis conducted in the Seguimiento Universidad de Navarra (SUN) as a practical example of the recommended methodology proposed by Knol and Vanderweele (Table 1).12 This analysis not only demonstrates the interrelatedness of diet and PA as two independent causal factors of mortality, but also helps identify to whom this combination may offer the greatest benefit as an intervention at the public health level. If an interaction is defined as the situation in which the effect of one exposure on an outcome differs across the strata of another exposure, the risk differences vary across strata, then the presence of interaction implies that effect of two exposures is different than the mere sum or multiplication of the individual effects.13 In this article we addressed the mechanistic or causal interaction created when two potential causal risk factors participate in the same causal mechanism, producing either a synergism or antagonism between factors on disease risk or death.
Reporting interactions on the additive scale is uncommon in standard epidemiologic reports. Current explanations as to why interactions may not be reported in greater detail include space constraints, word limits, or editorial intervention.14 Moreover, interactions on combined lifestyle factors are rarely a primary objective nor an initially intended analysis in most studies.5,15,16 However, the inclusion of these analyses provides essential information on the potential public health impact and causal structure of combined effects of different relevant exposures.14 Thus, more research is needed that report data on interactions as part of the primary hypothesis evaluated. Our comprehensive review observed a total of four studies as of May 21, 2020, that studied the combined effect of the MedDiet and PA on mortality, of which only one study reported p-values for interaction on the multiplicative scale. Our analysis was an extension to these findings by Alvarez-Alvarez et al. who interpreted, but did not evidence, the existence of a synergism, beyond additivity, but not beyond multiplicativity, equivalent to the mere multiplication of relative effects.9
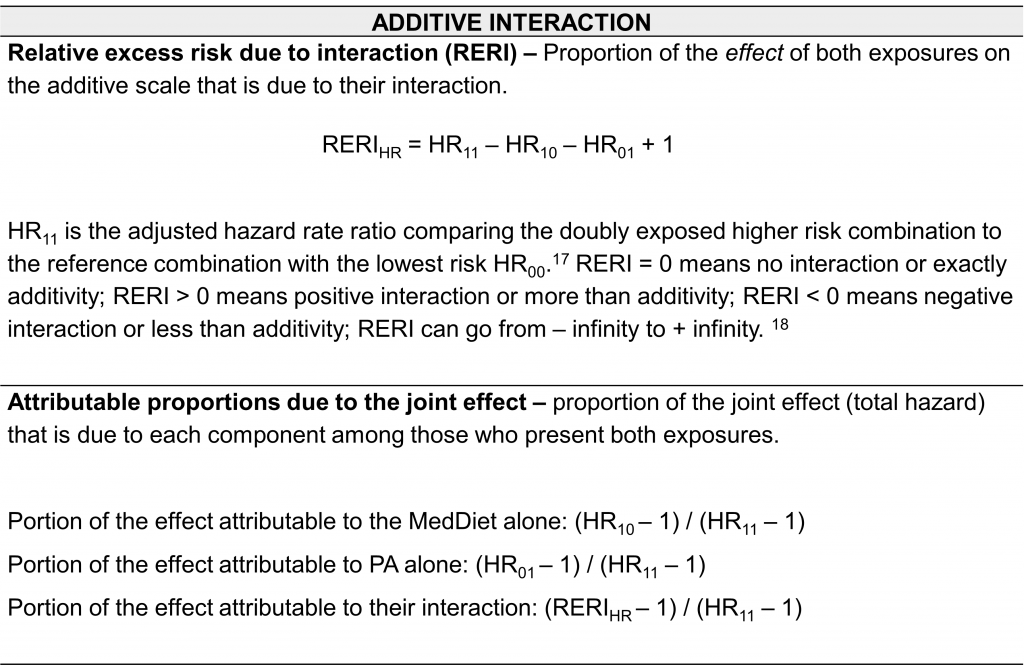
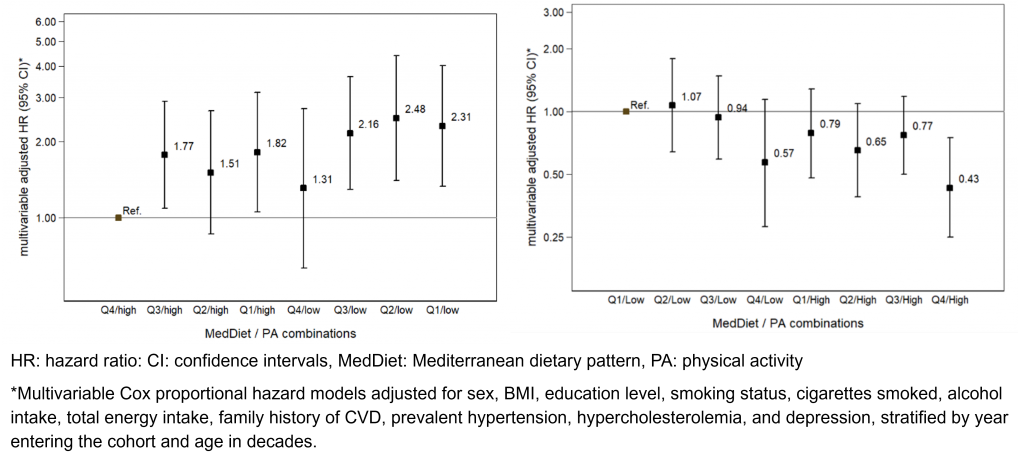
A key differentiation between these studies and our comprehensive interaction analysis was the recoding of preventive factors into risk factors for the correct estimation of additive interactions. We used Trichopoulou’s 9-item MedDiet score and an 8-item PA score to capture holistic measures of these dynamic multicomponent exposures. Combinations of both exposures were created with a contingency table for quartiles of MDS (Q4: high adherence to Q1: low adherence) and dichotomous PA scores (high: 4-8 points and low: 0-3 points). Interactions were analyzed according to the methodology proposed by Knol and Vanderweele by studying the single and joint effects of the exposures followed by an interaction analysis on both the multiplicative and additive scales.12,19
Our findings evidenced that the potential synergism between the MedDiet and PA is most likely beyond additivity, but below multiplicativity, in line with the conclusion first inferred by Alvarez-Alvarez et al. The combined effect of low MDS and low PA was associated with an even greater increased risk than the individual effects themselves, compared to the high MDS and high PA combination (Figure 1). According to our data, we quantified the effect due to the interaction was 36% of the total joint effect. Hence, the subgroup with low MedDiet adherence and low PA would benefit from an intervention targeting both habits simultaneously to reduce the risk posed by this synergism. However, the measures of interaction were not statistically significant, even when using continuous variables, most likely due to the statistical power, which must be greater than that required for a multivariable analysis. Moreover, one must bear in mind, the effect of the interaction varies according to the prevalence of the two exposures and the outcome within a given subgroup. Hence, the public health implications of the MedDiet and PA depend on the proportion of the population in which these factors occur jointly and the case distribution of the given outcome reported.20 Similarly, from a more applicable perspective to public health, increasing risk reductions were observed across combinations of MDS and PA on protective scales.
More studies on interactions are needed to fill the current research gap in nutritional epidemiology regarding quantifying interactions between lifestyle factors. The mechanism by which individual components interact is complex, suggesting the use of interaction analysis as an essential statistical method to complement frequently reported joint effects. Studying combinations of lifestyle factors is relevant for understanding the impact these multifaceted and interrelated habits have on individual and population health, as well as provide key insight for implementing successful multicomponent lifestyle interventions.22–27 Furthermore, other dietary patterns should be studied for greater generalizability and a meta-analysis of the effect attributed to the interaction between the MedDiet and PA would provide stronger evidence. These analyses are critical to providing high-quality evidence as interest grows in studying overall lifestyle patterns on health.
Summary based on the article: “The Mediterranean diet and physical activity: better together than apart for the prevention of premature mortality”. Hershey, M. S., Martínez-González, M. Á., Álvarez-Álvarez, I., Martínez Hernández, J. A., & Ruiz-Canela, M.. Published in the British Journal of Nutrition. 2021. doi:10.1017/S0007114521002877

Maria Soledad Hershey 
Miguel Ruiz-Canela 
Maria Soledad Hershey has a bachelors and master’s degree in human nutrition and dietetics from the University of Navarra in Pamplona, Spain. She is currently finishing her PhD in nutritional epidemiology in the Department of Preventive Medicine and Public Health at the same institution. Her research focuses on the population impact of lifestyle factors for the primordial prevention of chronic disease and premature mortality. In particular, she aims to provide evidenced based recommendations centered around the traditional Mediterranean lifestyle. As part of her predoctoral training Maria completed a research stay with Dr. Stefanos Kales at the Harvard T.H. Chan School of Public Health where she worked on two studies conducted within the Feeding America’s Bravest trial in US career firefighters. She looks forward to continuing working with this population at particularly high CVD risk, in which more research and lifestyle interventions are needed to reduce the burden from chronic disease among this critical working population.
Miguel Ruiz-Canela, PharmD, MPH, PhD, is Professor of Preventive Medicine and Public Health at the University of Navarra. He has been working for more than 20 years in the field of Nutritional Epidemiology, more specifically on the effect of lifestyle, including nutrition and physical activity, on several chronic diseases, mainly cardiovascular disease, obesity and type-2 diabetes. He has worked with the SUN cohort, and several intervention studies including the PREDIMED and PREDIMED-Plus trials. Currently, he is co-PI of a secondary prevention trial of atrial fibrillation with Mediterranean Diet (PREDIMAR study) and co-PI of an NIH-founded project on lifestyle interventions, metabolites, microbiome and diabetes risk. He is also involved in several projects related to Culinary Medicine including Dr. PED-Chef, SUKALMENA trial and n-CHEFS study. He has published more than 250 publications with an H-index of 39 (https://publons.com/researcher/1089901/miguel-ruiz-canela-phd-mph/)
References
- Meulenberg CJW. Health benefits induced by adherence to the Mediterranean lifestyle components diet and physical activity. Ann Kinesiol. 2019;10(1):15-30. doi:10.35469/ak.2019.175
- Ding EL, Hu FB. Commentary: Relative importance of diet vs physical activity for health. Int J Epidemiol. 2010;39(1):209-211. doi:10.1093/ije/dyp348
- Willett WC, Sacks F, Trichopoulou A, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6):1402S-1406S. Accessed August 9, 2021. https://academic.oup.com/ajcn/article/61/6/1402S-1406S/4651234
- Bach-faig A, Berry EM, Lairon D, et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011;14. doi:10.1017/S1368980011002515
- Loprinzi PD, Smit E, Mahoney S. Physical Activity and Dietary Behavior in US Adults and Their Combined Influence on Health. Mayo Clin Proc. 2014;89(2):190-198. doi:10.1016/j.mayocp.2013.09.018
- Martinez-Lacoba R, Pardo-Garcia I, Amo-Saus E, Escribano-Sotos F. Mediterranean diet and health outcomes: a systematic meta-review. Eur J Public Health. 2018;28(5):955-961. doi:10.1093/eurpub/cky113
- Galbete C, Schwingshackl L, Schwedhelm C, Boeing H, Schulze MB. Evaluating Mediterranean diet and risk of chronic disease in cohort studies: an umbrella review of meta-analyses. Eur J Epidemiol. 2018;33(10):909-931. doi:10.1007/s10654-018-0427-3
- Soltani S, Jayedi A, Shab-Bidar S, Becerra-Tomás N, Salas-Salvadó J. Adherence to the Mediterranean Diet in Relation to All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv Nutr. 2019;10(6):1029-1039. doi:10.1093/advances/nmz041
- Alvarez-Alvarez I, Zazpe I, Pérez de Rojas J, et al. Mediterranean diet, physical activity and their combined effect on all-cause mortality: The Seguimiento Universidad de Navarra (SUN) cohort. Prev Med (Baltim). 2018;106(Supl. 1):45-52. doi:10.1016/j.ypmed.2017.09.021
- Pronk NP, Anderson LH, Crain AL, et al. Meeting recommendations for multiple healthy lifestyle factors. Am J Prev Med. 2004;27(2):25-33. doi:10.1016/j.amepre.2004.04.022
- Ding D, Rogers K, van der Ploeg H, Stamatakis E, Bauman AE. Traditional and Emerging Lifestyle Risk Behaviors and All-Cause Mortality in Middle-Aged and Older Adults: Evidence from a Large Population-Based Australian Cohort. Tumwine JK, ed. PLOS Med. 2015;12(12):e1001917. doi:10.1371/journal.pmed.1001917
- Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514-520. doi:10.1093/ije/dyr218
- VanderWeele TJ, Lash TL, Rothman KJ. Analysis of Interaction. In: Modern Epidemiology. Fourth Edi. Wolters Kluwer; 2021:619-653.
- Knol MJ, Egger M, Scott P, Geerlings MI, Vandenbroucke JP. When One Depends on the Other. Epidemiology. 2009;20(2):161-166. doi:10.1097/EDE.0b013e31818f6651
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495-1499. doi:10.1016/j.ijsu.2014.07.013
- Edwards MK, Loprinzi PD. Physical activity and diet on atherogenic index of plasma among adults in the United States: mediation considerations by central adiposity. Eur J Clin Nutr. 2018;72(6):826-831. doi:10.1038/s41430-017-0066-x
- Li R, Chambless L. Test for Additive Interaction in Proportional Hazards Models. Ann Epidemiol. 2007;17(3):227-236. doi:10.1016/j.annepidem.2006.10.009
- Rothman KJ. Modern Epidemiology. 1st ed. Little, Brown; 1986.
- VanderWeele TJ, Knol MJ. A Tutorial on Interaction. Epidemiol Method. 2014;3(1):33-72. doi:10.1515/em-2013-0005
- Rothman KJ, Greenland S, Walker AM. Concepts of interaction. Am J Epidemiol. 1980;112(4):467-470. doi:10.1093/oxfordjournals.aje.a113015
- Zhang Y-B, Pan X-F, Chen J, et al. Combined lifestyle factors, all-cause mortality and cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. J Epidemiol Community Health. Published online September 5, 2020:jech-2020-214050. doi:10.1136/jech-2020-214050
- Hamer M, Bates CJ, Mishra GD. Multiple Health Behaviors and Mortality Risk in Older Adults. J Am Geriatr Soc. 2011;59(2):370-372. doi:10.1111/j.1532-5415.2011.03258.x
- Byun W, Sieverdes JC, Sui X, et al. Effect of Positive Health Factors and All-Cause Mortality in Men. Med Sci Sport Exerc. 2010;42(9):1632-1638. doi:10.1249/MSS.0b013e3181d43f29
- Li Y, Pan A, Wang DD, et al. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation. 2018;138(4):345-355. doi:10.1161/CIRCULATIONAHA.117.032047
- Perak AM, Ning H, Khan SS, et al. Associations of Late Adolescent or Young Adult Cardiovascular Health With Premature Cardiovascular Disease and Mortality. J Am Coll Cardiol. 2020;76(23):2695-2707. doi:10.1016/j.jacc.2020.10.002
- Gong Q, Zhang P, Wang J, et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. lancet Diabetes Endocrinol. 2019;7(6):452-461. doi:10.1016/S2213-8587(19)30093-2
- Fernández-Alvira JM, Fernández-Jiménez R, de Miguel M, et al. The challenge of sustainability: Long-term results from the Fifty-Fifty peer group-based intervention in cardiovascular risk factors. Am Heart J. 2021;240:81-88. doi:10.1016/J.AHJ.2021.06.006

