By Fredrik Åberg
Fatty liver disease (FLD), the accumulation of fat in liver cells, presently affects around 25% of adults (1). Of these, one fifth suffer from the more severe form of FLD, namely steatohepatitis, which over time can progress to liver cirrhosis, liver cancer and end-stage liver disease.
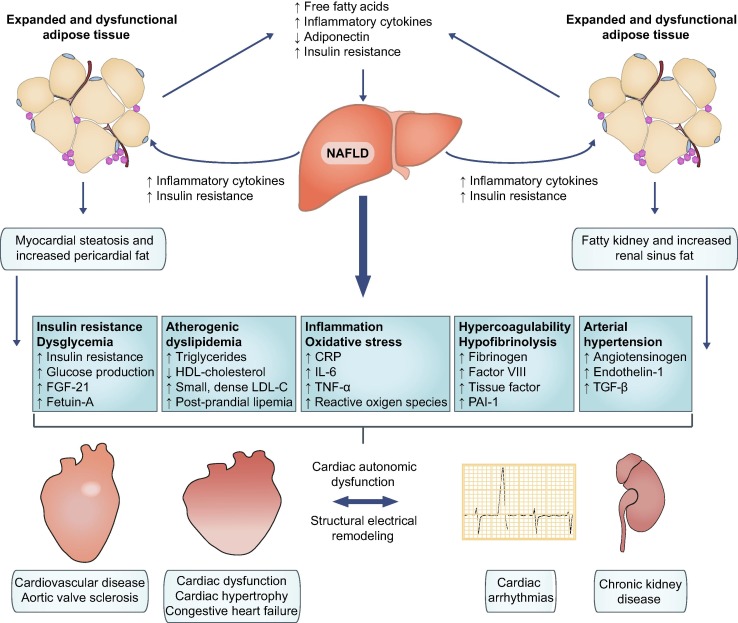
FLD is most often associated with abdominal obesity, insulin resistance, and the metabolic syndrome (non-alcoholic fatty liver disease, NAFLD). Other causes of FLD include hazardous alcohol consumption, genetics, certain medications, parenteral nutrition and viral hepatitis.
Alcohol intake of less than 30 grams of pure ethanol among men or less than 20 grams among women is generally not considered to cause liver fat accumulation, but the effects of such light-moderate alcohol use on the background of pre-existing obesity-related FLD are controversial.
Numerous studies on individuals with NAFLD have shown an association between light-moderate alcohol consumption, particularly wine, and milder liver disease compared to total alcohol abstinence (2-4). It has been suggested that the beneficial effects of light alcohol use on insulin sensitivity can lead to a reduction in the amount of fat in the liver. However, the hepatotoxic effects of alcohol are not limited to simple fat accumulation alone, and there is conflicting clinical evidence on the effects on the liver of light-moderate alcohol consumption. Studies reporting liver-protective effects of alcohol are limited by a number of potential biases. For instance, they have been conducted mainly in cross-sectional settings (exposure and outcome variables are measured simultaneously), with insufficient adjustment for confounding factors such as lifestyle, socioeconomic status, and co-morbidity, and the outcome variables used in these studies most often represent surrogate markers such as steatosis or liver enzymes. People with previous drinking who later stopped drinking (current abstainers) are often not separated from lifetime abstainers. In addition, underestimation of alcohol intake is particularly common among people who already know they have liver disease (cross-sectional studies).
In a recent longitudinal Finnish study, we were able to overcome many of these limitations of earlier studies (5). Combining data from the Finnish FINRISK 1992-2012 and Health 2000 population surveys with data from national mandatory registers for hospitalizations, cancer and death related to liver disease enabled analyzes on the effects of alcohol use on the risk of incident advanced clinical liver disease. We excluded persons who consumed> 50 grams of alcohol per day, current abstainers, and those with viral hepatitis (at baseline or during follow-up) or baseline severe liver disease. Analyzes were adjusted for various risk factors, lifestyle factors and socioeconomic status.
In the combined cohort of the more than 27,000 persons, 8345 had NAFLD at baseline (defined as a Fatty Liver Index > 60). We found no liver-beneficial effects of light-moderate alcohol intake. On the contrary, even low alcohol consumption increased the risk of advanced liver disease. Among persons with NAFLD, a daily intake of 10 to 19 grams of any type of alcohol doubled the risk of advanced liver disease compared to non-drinkers. A similar risk increase was seen already at alcohol intake of less than 10 grams per day when the consumption was in the form of non-wine beverages. In contrast, wine drinking with total average intake of less than 25 grams per day of ethanol did not significantly raise the risk of advanced liver disease.
Regarding the risk for cardiovascular disease (CVD), we found a tendency towards reduced risk with light-moderate alcohol intake even after multiple adjustments. This was sensitive to beverage type with a larger risk reduction seen in preferential wine drinkers than preferential beer or spirits drinkers. In contrast, light drinking raised the risk for cancer, without any clear effect modification from the fraction of wine. We found a J-shaped relationship between alcohol use and all-cause mortality with a maximal risk reduction of 21% at alcohol intake of 0-9 g/day in the fully adjusted model. Larger risk reductions for death were again seen in preferential wine drinkers than in non-wine drinkers. Alcohol intake above 30 g/day was associated with increased mortality. The J-shaped relationship between alcohol and mortality was only evident in never smokers, suggesting that smoking modifies the relationship between alcohol and risk of death.
Taken together, among non-smokers with NAFLD, the absolute risk increases for liver cirrhosis conferred by drinking 1-2 standard glasses of wine per day seems minimal, so this may not need to be prohibited in the average individual with NAFLD without advanced liver fibrosis. In NAFLD with advanced liver fibrosis or particular risk for progressive liver disease, however, complete alcohol abstinence seems warranted. The clinical implications of the J-shaped association between alcohol and incident CVD and death in never smokers remain unclear, and needs to be balanced against an increased risk for cancers. From a holistic point of view, there are more effective and safer means to reduce CVD risk than by alcohol use, and given the elevated risk estimates for advanced liver disease and cancer in general, light-moderate alcohol drinking cannot be encouraged in people with NAFLD.

Fredrik Åberg
Email: fredrik.aberg@hus.fi
PERSONAL DATA
Name Fredrik Oskar Åberg
Date of birth 14.03.1981
EDUCATION
2018 Helsinki University, Faculty of Medicine, Adjunct professor (docent)
2015 Helsinki University, Faculty of Medicine, Specialist in gastroenterology
2010 Helsinki University, Faculty of Medicine, Doctor of medical sciences (PhD)
2007 Helsinki University, Faculty of Medicine, Licentiate of medicine
2000 Brändö Gymnasium, higher school certificate
WORK EXPERIENCE
08/2017 – Sahlgrenska university hospital (Sweden), Transplant Institute
10/2015 – HUCS Meilahti hospital, Transplantation and Liver Surgery Clinic
04/2013 – 10/2015 HUCS Meilahti hospital, Deparment of Gastroenterology
01/2013 – 03/2013 HUCS Meilahti hospital, Transplantation and Liver Surgery clinic
01/2012 – 12/2012 HUS Maria (Malm) hospital, Department of Internal medicine
12/2009 – 01/2012 Diacor, Helsinki, General medicine
2007 – 2010 HUS Porvoo Hospital, Porvoo, Department of Internal medicine
02/2008 – 12/2008 Porvoo Health Center, General medicine
06-08/2006 HUS Tammisaari Hospital, Department of Emergency medicine
06-08/2005 HUCS Surgical Hospital, Department of Anaesthesiology
ADDITIONAL ACTIVITES
2015 – Finland’s representative in United European Gastroenterology (UEG) “Friends of
Young Talent Group”
2014 – 2016 Research foundation for gastrointestinal diseases, commissioner
2015 – 2017 Finland’s representative in Scandiatransplant Association
2014 – 2015 HUCS Endoscopy team, member and Department of Gastroenterology team, member
01/2002 – Medicinarklubben Thorax r.f. (student organisation for medical students)
INVITED TALKS AT INTERNATIONAL MEETINGS: 4 times (ILTS, British Transplant
Society, Astellas Network Meeting, Nordic Hemophilia days, Nordic Liver Transplant
Group 25yr Anniversary Symposium)
INVITED TALKS AT NATIONAL MEETINGS: 37 times
ORAL ABSTRACT PRESENTATIONS: 13 times at key international meetings including EASL
International Liver Congress’ grand session, ILTS, ESOT, TTS, STS, ELITA
REVIEWER FOR MANUSCRIPTS IN PEER-REVIEWED JOURNALS
52 reviews in 25 different journals, including Gastroenterology, Hepatology, American
Journal of Transplantation, Liver International, Liver Transplantation
Ongoing reviewer for Centre for Evidence in Transplantation, Transplant Library
INTERNATIONAL AWARDS
EASL travel grant 2013
EASL International Liver Congress travel and abstract award 2017 and oral
presentation at Grand Session
Finnish nominee for UEG Rising star award 2018 and 2019
RESEARCH GRANTS
Mary och Georg Ehrnrooth foundation (2009, 2017, 2018), Stockmann foundation (2016), Finska
Läkaresällskapet (2009, 2014, 2015, 2016, 2017, 2018), Finnish-Norwegian medical society (2014,
2017), Liv och Hälsa foundation (2007, 2008, 2009, 2010, 2016, 2017), Perklen foundation (2009,
2014), Scandiatransplant (2012), Maud Kuistila memorial fund (2009), Biomedicum foundation
(2009), Finnish transplantation society (2008)
OTHER: GCP training PharmaSchool certificate 23.8.2016
References
- Younossi ZM. J Hepatol. 2019;70(3):531-544
- Moriya A et al. Aliment Pharmacol Ther. 2011;33(3):378-388
- Dunn W et al. J Hepatol. 2012;57(2):384-391
- Mitchell T et al. Am J Gastroenterol. 2018;113(10):1484-1493
- Åberg F et al. Hepatology. 2019 Jul 19 (Epub ahead of print)

