By Sohaib Haseeb, Bryce Alexander, Ricardo Lopez Santi, Adrian Baranchuk
Wine has been consumed for years as a social drink, attracting great interest during recreational and personal occasions (Haseeb et al., 2017; Haseeb et al., 2018). In 2017, global wine consumption was 243 million hectoliters (mhl), with the United States being the largest global consumer (32.6 mhl) followed by France (27.0 mhl) and Italy (22.6 mhl) (International Organisation of Vine and Wine, 2017). Despite the wide accessibility of wine, its excessive intake is an established risk factor for premature death and disability. The excessive intake of wine and alcohol has been found to contribute to liver cirrhosis (Rehm et al., 2010), sudden cardiac death (Wannamethee & Shaper, 1992), alcoholic cardiomyopathy (Lazarević et al., 2000), and cardiac rhythm disorders, namely atrial fibrillation (Voskoboinik et al., 2016). However, wine has historically garnered attention as a healthy beverage. Epidemiological evidence has accumulated in support of a negative correlation between the light-to-moderate consumption of wine and ischemic heart disease (IHD) mortality. Despite many epidemiological studies reaching similar conclusions, the causal nature of these findings remains an open question. Some studies have observed similar effects with the consumption of beer and spirits, while others have reported that alcohol as a whole is protective and that the type of drink is not of importance (Roerecke & Rehm, 2014). This post highlights the most important aspects of wine and cardiovascular health, relevant metrics of calculation, current guidelines and discrepancies, and attitudes and perceptions of healthcare practitioners.
The French Paradox
Wine became a drink of scientific intrigue in the late 20th century after studies found that its sustained intake at light-to-moderate amounts may possibly confer cardioprotective effects (Baranchuk et al., 2018b). A negative correlation between the light-to-moderate intake of wine and IHD mortality was described using epidemiological studies, first appearing in the 1960s. This phenomenon was eventually coined the French Paradox after epidemiologists Serge Renaud and Michel de Lorgeril who observed a relatively low rate of IHD mortality in France despite a consumption of a diet rich in cholesterol and saturated fats (Renaud & de Lorgeril, 1992). The authors attributed the cardioprotective effects of this phenomenon to the moderate intake of alcoholic beverages, especially red wine, which was highly consumed in the area. Drinking patterns, lifestyle characteristics, and dietary intake are all important factors that need to be considered in order to obtain a healthy cardiovascular profile.
Bioactive constituents of wine
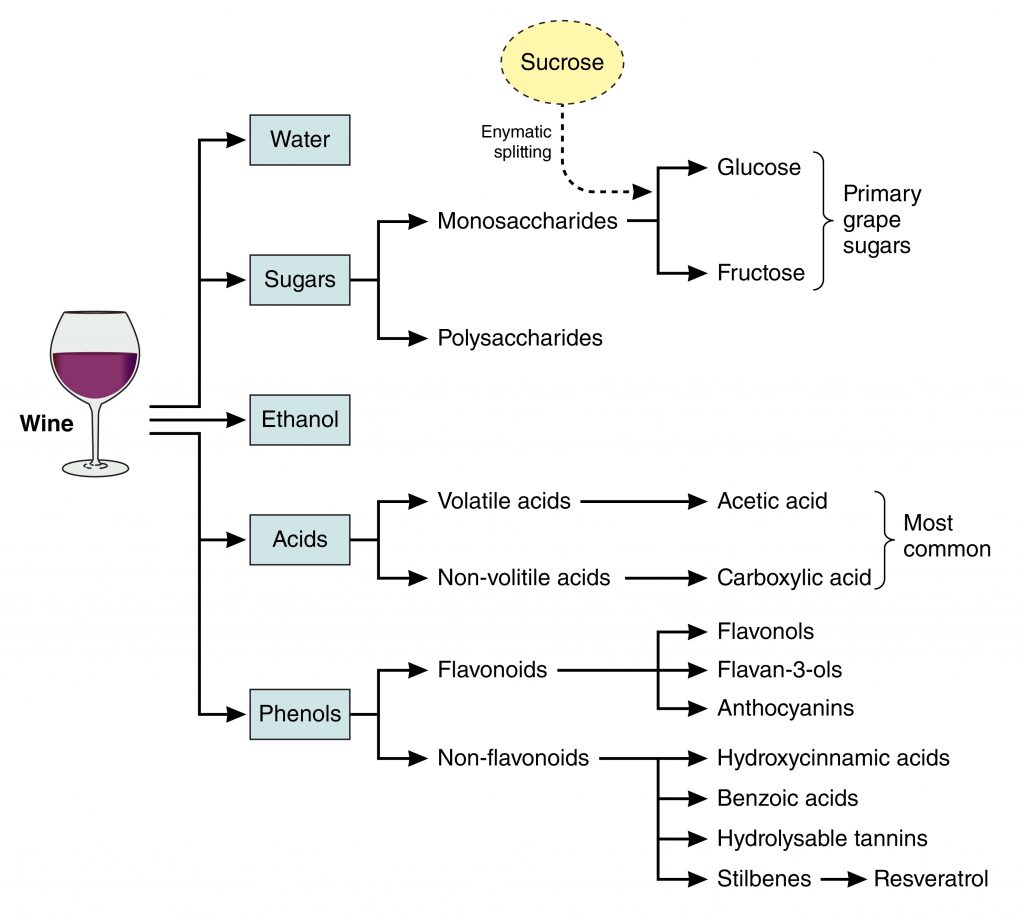
Wine is composed of >500 constituents. The major constituents by weight are water and ethanol. Other constituents of importance are sugars, acids, other alcohols, and phenolics (Haseeb et al., 2018). The detailed chemical composition of wine can be viewed in Figure 1. The ethanol and polyphenols are considered to be the bioactive constituents of wine with regards to cardiovascular health. They are of particular interest for their potential antioxidant and anti-inflammatory properties.
Wine phenolics can be divided into two categories: the flavonoids and non-flavonoids. Flavonoids are plant-based compounds that are naturally present in grapes and wine. Flavonoids from red wine have been found to inhibit low-density-lipoprotein (LDL) oxidation (Nigdikar et al., 1998), prevent endothelial dysfunction (Perez-Vizcaino et al., 2006), and reduce atherosclerosis development (Mano et al., 1996). Non-flavonoids in wine include hydrolysable tannins, hydroxycinnamates, carboxylic acid derivatives, and resveratrol. The cardiovascular effects of resveratrol have largely been reported in animal models, with limited but increasing studies in humans. Several animal studies have shown that the intake of dietary resveratrol lowers LDL cholesterol, triglycerides, but increases HDL cholesterol (Ahn et al., 2008; Do et al., 2008; Penumathsa et al., 2007). Clinical studies have been more variable, finding that the effect cannot be attributed to resveratrol alone. In general, preclinical and clinical studies have shown interesting results with regards to resveratrol and cardiovascular health.
What constitutes a “standard drink”?
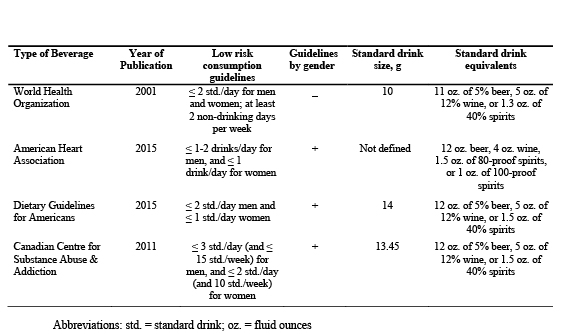
Alcohol guidelines are reported in units called standard drinks (SD) in order to quantify alcohol intake, monitor associated risks, and encourage safe drinking practices. The World Health Organization’s (WHO) Alcohol Use Disorders Identification Test (AUDIT) defines 1 SD to equal 10 g of pure ethanol (Babor & Higgins-Biddle, 2001). The US Dietary Guidelines define 1 SD to equal 14 g of pure ethanol (US Department of Health and Human Services, 2015), and the Canadian Centre for Substance Abuse and Addiction (CCSA) define 1 SD to equal 1 g of pure ethanol (Butt et al., 2011) (Table 1). The definition of 1 SD is highly variable and discrepant between countries (Baranchuk et al., 2018a).
Drinking guidelines: What do the cardiovascular societies say?
Various societies have introduced drinking guidelines for current drinkers to promote a safe drinking culture. The WHO recommends low-risk alcohol intake of ≤ 2 SD per day with at least 2 non-drinking per week (Babor & Higgins-Biddle, 2001). The American Heart Association recommends alcohol in moderation; an average of ≤ 1-2 drinks/day for men, and ≤ 1 drink/day for women (American Heart Association, 2015). The US Dietary Guidelines recommend ≤ 2 SD per day for men and ≤ 1 SD per day for women (US Department of Health and Human Services, 2015). The CCSA recommends ≤ 3 SD per day (and ≤ 15 SD per week) for men, and ≤ 2 SD per day (and 10 SD per week) for women (Butt et al., 2011) (Table 1). Low-risk recommendations of alcohol intake have been defined in at least 37 countries. Despite the increased awareness of alcohol and its adverse effects on health, drinking guidelines are not well-known to general consumers (Buykx et al., 2018).
Attitudes and recommendations of healthcare providers
There are many misconceptions regarding the risks and benefits of alcohol intake in the public arena (Baranchuk et al., 2017; Haseeb et al., 2018). Healthcare providers are well positioned to counsel their patients regarding appropriate levels of alcohol intake and its risks and benefits of consumption. However, there is little direct evidence to ascertain their attitudes and recommendations towards alcohol and cardiovascular health. Our group conducted a national study in Argentina to investigate this question (Lopez Santi et al., 2018). The results showed that Argentine physicians had variable perceptions of alcohol as it relates to cardiovascular health. Argentine physicians were not satisfied with their knowledge of the drinking guidelines or its reported metric units, particularly SD. The existence of these knowledge gaps suggests a need to optimize educational resources for healthcare providers.
Conclusions
Despite the excessive intake of wine being a risk factor to general and cardiovascular health, it is a popular beverage among drinking adults. There are noted beneficial effects of a controlled and sustained light-to-moderate intake to be beneficial for the cardiovascular profile, although this evidence is inconsistent. Drinking guidelines for current drinkers are in place to promote safe drinking.
Those interested in a longer length report can download the working paper at:
https://www.sciencedirect.com/science/article/pii/S1050173818301142

Sohaib Haseeb is a student at Queen’s University, Kingston, Ontario, Canada studying Life Sciences.

Dr. Bryce Alexander received his M.D. from Queen’s University in 2018. He is currently a first year internal medicine resident (PGY-1) at Queen’s University in Kingston, Ontario, Canada.

Dr. Ricardo Lopez Santi is a native of La Plata city, Argentina. He obtained his M.D. from La Plata University in 1980 and is currently a consultant cardiologist and specialist in health systems and social security at ISALUD University. Dr. Lopez Santi served as the Director of non-communicable diseases at the Health Ministry of Buenos Aires from 2007 to 2012. He was the President of the scientific committee at the XXVII Congress of the Argentine Federation of Cardiology in 2009. He served as the President of the Argentine Federation of Cardiology (FAC) from 2010 to 2011, and is currently a member of the consultant board of the FAC. In 2015, Dr. Lopez Santi was promoted to the Chief of promotion and prevention at the Italian Hospital of La Plata city. He is the Chair Professor of Cardiovascular prevention, Medical school, Santiago del Estero. He is a Fellow of the American College of Cardiology (FACC), Chair of the Community council of the Interamerican Society of Cardiology, and the elected Governor of the International Society of Cardiovascular Pharmacotherapy (ISCP) for Argentina. Dr. Lopez Santi has participated in more than 20 national (EMECO, Raices) and international research projects with support from organizations such as NIH (WARCEF) European Economic Community (FOCUS regional coordinator) and various pharmaceutical industries (Origin, Value, Navigator, Shift, Atmosphere, Rewind, Compass, Fourier, Prominent). He is a co-author of the book “Cardiometabolism, from the physiopathology to the therapeutic” 2nd edition. For 12 consecutive years, Dr. Lopez Santi has spearheaded a national campaign of promotion called “One hundred thousand hearts”.
Dr. Adrian Baranchuk, a native of Buenos Aires, Argentina, obtained his MD from the University of Buenos Aires in 1990. After qualifying in Internal Medicine and Cardiology (1995), he completed a Clinical Fellowship in Cardiac Electrophysiology (1997). In 2002 he immigrated to Spain for a Research Fellow. Dr. Baranchuk was appointed as a Clinical Fellow in Electrophysiology at McMaster University in September 2003. Dr. Baranchuk was appointed as an Assistant Professor of Medicine at Queen’s University (2006), promoted to Associate Professor in 2010 and to Full Professor in 2016 (with Tenure). He has founded the EP Training Program in 2007. He is a member of numerous editorial boards (Europace, Annals of Noninvasive Electrocardiology, etc.) and reviewer of several journals. He is currently the Editor-in-Chief of the Journal of Electrocardiology. The recipient of a teaching award (Outstanding Contribution in the Core Internal Medicine Program 2009) and 2014 awarded with the prestigious “Faculty of Health Sciences Education Award”. Dr. Baranchuk was awarded with the “Golden Caliper Award” from the SOLAECE (Latin American Society of Pacing and Electrophysiology) for his outstanding contributions to science in 2014 and with the “ISHNE Junior Investigator Award” in April 2015. In 2016 he was distinguished with the “10 Most Influential Hispanic-Canadian Award” from the Hispanic business.ca and TD Bank. He was recently awarded with the “David Ginsburg Mentorship Award” in December 2017. His first book, Atlas of Advanced ECG Interpretation (REMEDICA, UK) represents a big collaboration effort from well-recognized electrophysiologists of all around the world. His second book Left Septal Fascicular Block was released by SPRINGER in 2016 and his iBook “Electrocardiogrpahy in Pracitice: What to do?” has been number 1 in iTunes for several weeks and downloaded more than 1100 times in about 6 months (2016). His last book “Interatrial Block and Supraventricular Arrhythmias: Clinical Implications of Bayes’ Syndrome” was released in January 2017 by CARDIOTEXT. His last book “Clinical Arrhythmology 2nd Edition” was released in July 2017 by Willey. His next book, “Brugada Phenocopy: The Art of Recognizing the Brugada ECG Pattern” was released by ELSEVIER in March 2018.
He has published more than 520 articles in well-recognized international journals (463 in Pubmed), 50 book chapters and presented more than 225 abstracts. He is the President of the International Society of Electrocardiology (ISE) for the period 2017-2019. He is currently serving as Canadian Vice President of the Interamerican Society of Cardiology (2017-2019). He has mentored more than 100 students and residents and his publications usually include a Med Student or resident as first author. He is the current Director of the Critical Enquiry course at Queen’s University. He has been elected Member of the Electrophysiology Section Leadership Council of the American College of Cardiology (2017-2020). He is in charge of organizing the ECG module for the trainee day and the ECG Workshops during the Canadian Cardiovascular Congress. He chairs the Annual Cardiovascular Symposium at Queen’s University. He lives in Kingston, Ontario, Canada with his wife Barbara and his daughter, Gala.
References:
- Ahn, J., Cho, I., Kim, S., Kwon, D., & Ha, T. (2008). Dietary resveratrol alters lipid metabolism-related gene expression of mice on an atherogenic diet. Journal of Hepatology, 49(6), 1019–1028. doi:10.1016/j.jhep.2008.08.012
- American Heart Association. (2015, January 12). Alcohol and Heart Health. Retrieved from http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Nutrition/Alcohol-and-Heart-Health_UCM_305173_Article.jsp#.WtlLL4jwZPY
- Babor, T. F., & Higgins-Biddle, J. C. (2001). Brief intervention for hazardous and harmful drinking: a manual for use in primary care. Retrieved from http://apps.who.int/iris/bitstream/10665/67210/1/WHO_MSD_MSB_01.6b.pdf
- Baranchuk, A., Alexander, B., & Haseeb, S. (2017, December 2). Drinking red wine is good for you — or maybe not. Retrieved from https://www.washingtonpost.com/national/health-science/drinking-red-wine-is-good-for-you–or-maybe-not/2017/12/01/49f55e7a-cbd3-11e7-aa96-54417592cf72_story.html
- Baranchuk, A., Haseeb, S., & Alexander, B. (2018a). Alcohol Consumption Guidelines: International Discrepancies and Variations. BMJ. https://www.bmj.com/content/361/bmj.k1630/rr-1
- Baranchuk, A., Haseeb, S., & Alexander, B. (2018b, February 13). Wine Consumption and Cardiovascular Health: An Expert Opinion. Retrieved from http://www.iscpcardio.org/expert-opinions/wine-consumption-and-cardiovascular-health-an-expert-opinion/
- Butt, P., Beirness, D., Gliksman, L., Paradis, C., & Stockwell, T. (2011). Alcohol and Health in Canada: A Summary of Evidence and Guidelines for Low-risk Drinking. Ottawa, ON: Canadian Centre on Substance Abuse.
- Buykx, P., Li, J., Gavens, L., Hooper, L., Gomes de Matos, E., & Holmes, J. (2018). Self-Reported Knowledge, Correct Knowledge and use of UK Drinking Guidelines Among a Representative Sample of the English Population. Alcohol and Alcoholism (Oxford, Oxfordshire). doi:10.1093/alcalc/agx127
- Do, G.M., Kwon, E.Y., Kim, H.J., Jeon, S.M., Ha, T.Y., Park, T., & Choi, M.S. (2008). Long-term effects of resveratrol supplementation on suppression of atherogenic lesion formation and cholesterol synthesis in apo E-deficient mice. Biochemical and Biophysical Research Communications, 374(1), 55–59. doi:10.1016/j.bbrc.2008.06.113
- Haseeb, S., Alexander, B., & Baranchuk, A. (2017). Wine and Cardiovascular Health: A Comprehensive Review. Circulation, 136(15), 1434–1448. doi:10.1161/CIRCULATIONAHA.117.030387
- Haseeb, S., Alexander, B., & Baranchuk, A. (2018). Response by Haseeb et al to Letter Regarding Article, “Wine and Cardiovascular Health: A Comprehensive Review.” Circulation, 137, 1880–1881. doi:10.1161/CIRCULATIONAHA.117.033086
- Haseeb, S., Alexander, B., Santi, R. L., Liprandi, A. S., & Baranchuk, A. (2018). What’s in wine? A clinician’s perspective. Trends in Cardiovascular Medicine, [Epub ahead of print]. doi:10.1016/j.tcm.2018.06.010
- International Organisation of Vine and Wine. (2017). OIV Statistical Report on World Vitiviniculture. Retrieved from http://www.oiv.int/public/medias/5479/oiv-en-bilan-2017.pdf
- Lazarević, A. M., Nakatani, S., Nesković, A. N., Marinković, J., Yasumura, Y., Stojicić, D., Miyatake, K., Bojić, M., Popović, A. D. (2000). Early changes in left ventricular function in chronic asymptomatic alcoholics: relation to the duration of heavy drinking. Journal of the American College of Cardiology, 35(6), 1599–1606.
- Lopez Santi, R., Haseeb, S., Alexander, B., D′Ovidio, A., Gimenez, S., Secotaro, C., Martinez Demaria, D., Pupi, L. M., Costantini, S., Piskorz, D., Amarilla, A., Lorenzatti, A., Gutierrez, N., Hopman, W., Baranchuk, A. (2018). Attitudes and Recommendations of Physicians towards Alcohol Consumption and Cardiovascular Health: A Perspective from Argentina. Diseases, 6(3), 77. doi:10.3390/diseases6030077
- Mano, T., Masuyama, T., Yamamoto, K., Naito, J., Kondo, H., Nagano, R., Tanouchi,
- J., Hori, M., Inoue, M., Kamada, T. (1996). Endothelial dysfunction in the early stage of atherosclerosis precedes appearance of intimal lesions assessable with intravascular ultrasound. American Heart Journal, 131(2), 231–238.
- Nigdikar, S. V., Williams, N. R., Griffin, B. A., & Howard, A. N. (1998). Consumption of red wine polyphenols reduces the susceptibility of low-density lipoproteins to oxidation in vivo. The American Journal of Clinical Nutrition, 68(2), 258–265.
- Penumathsa, S. V., Thirunavukkarasu, M., Koneru, S., Juhasz, B., Zhan, L., Pant, R., Maulik, N. (2007). Statin and resveratrol in combination induces cardioprotection against myocardial infarction in hypercholesterolemic rat. Journal of Molecular and Cellular Cardiology, 42(3), 508–516. doi:10.1016/j.yjmcc.2006.10.018
- Perez-Vizcaino, F., Duarte, J., & Andriantsitohaina, R. (2006). Endothelial function and cardiovascular disease: Effects of quercetin and wine polyphenols. Free Radical Research, 40(10), 1054–1065. doi:10.1080/10715760600823128
- Rehm, J., Taylor, B., Mohapatra, S., Irving, H., Baliunas, D., Patra, J., & Roerecke, M. (2010). Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug and Alcohol Review, 29(4), 437–445. doi:10.1111/j.1465-3362.2009.00153.x
- Renaud, S., & de Lorgeril, M. (1992). Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet London Engl, 339(8808), 1523–1526.
- Roerecke, M., & Rehm, J. (2014). Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Medicine, 12, 182. doi:10.1186/s12916-014-0182-6
- US Department of Health and Human Services. (2015). Dietary Guidelines for Americans 2015–2020. Retrieved from https://health.gov/dietaryguidelines/2015/guidelines/appendix-9/
- Voskoboinik, A., Prabhu, S., Ling, L., Kalman, J. M., & Kistler, P. M. (2016). Alcohol and Atrial Fibrillation. Journal of the American College of Cardiology, 68(23), 2567–2576. doi:10.1016/j.jacc.2016.08.074
- Wannamethee, G., & Shaper, A. G. (1992). Alcohol and sudden cardiac death. British Heart Journal, 68(5), 443–448.